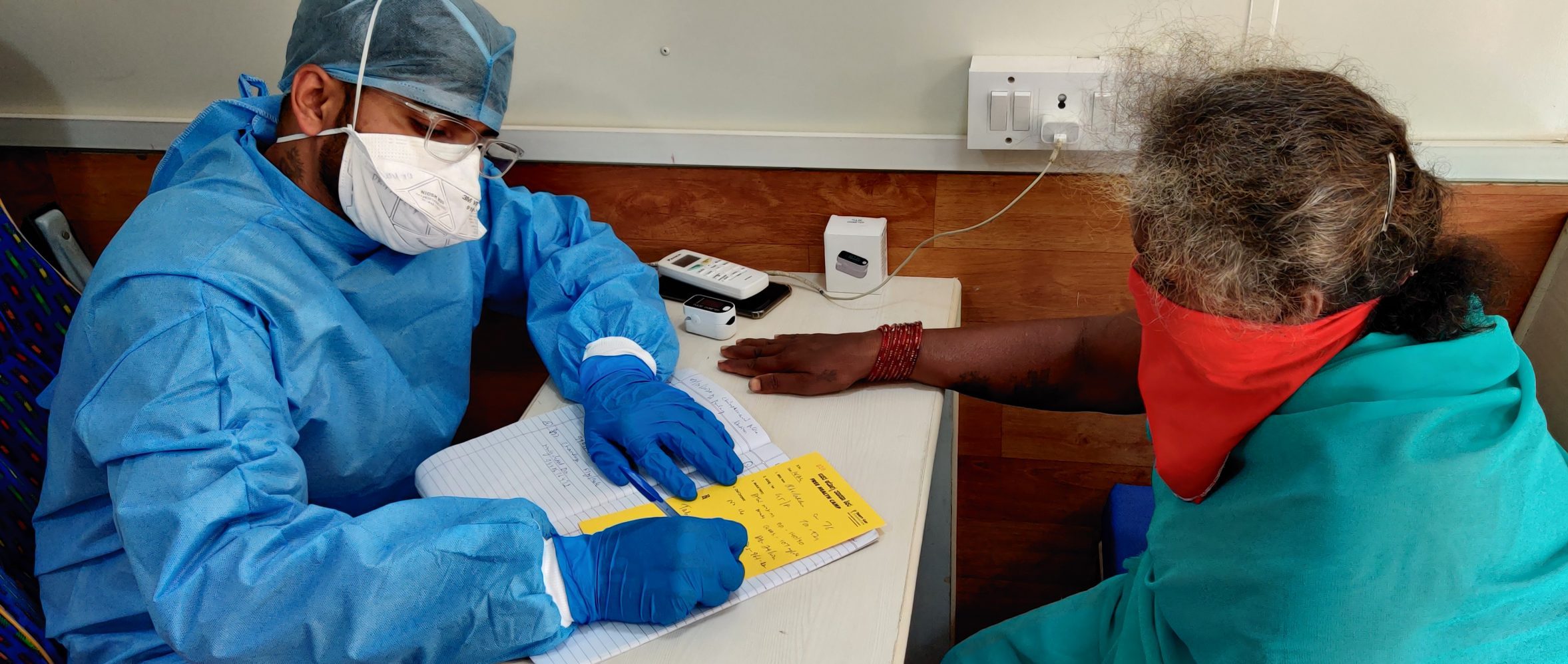
Image: Karnataka state, India. Trinity Care Foundation via Flickr
The COVID-19 pandemic and associated catastrophic financial burden: a tragedy still in the making
27 July 2021
Our colleagues from Oxford Policy Management, Rakesh Parashar and Ankita Mukherjee, describe the under-reported financial burden faced by everyday people and the growing health inequality in India.
This article has been cross-posted with kind permission from the original submission on the Health Policy and Planning Debated blog site.
Lost in the discourse and politics of containing the pandemic through strict implementation of COVID-19 guidelines, producing vaccines, creating public awareness, and an endless push and pull on the drugs to treat COVID-19, we seemingly have neglected something- the everyday people. Health systems are made for people, yet this pandemic is worsening social inequality. People living through the pandemic are more likely to fall sick and without health cover they face severe financial hardship. In a low-resource setting – amidst limited income, no health protection, and caring for the family – availing health services is a conscious decision, and often a low priority.
Any discussion on universal health coverage is incomplete if private health payments are not accounted for, yet this is largely missed during the biggest pandemic of modern history. Many additional families are now more likely to face catastrophic health expenditures (CHE) (read the WHO report on reducing CHE) due to COVID-19-related expenses. Seven months into the pandemic, we are yet to estimate the additional productivity costs of COVID-19 incurred by different population groups. Therefore, we remind the global health community to prioritise health financial-risk protection of families, failing to do so could potentially derail the economic-wellbeing and impact their future. In this blog post we highlight the case of India which has recorded the second-highest reported cases of COVID-19 globally by November 2020.
The case of India
India is one of the countries that spends the least on healthcare (see the 2019 National Health Profile). The enormous disparity in the wealth distribution between an urban and rural wage-earner adversely reflects their healthcare-seeking behaviours. The poor cannot afford to fall sick as it will only make them poorer- even in public facilities (see this BMC paper on the issue). 60% of the healthcare expenses in India are met by out-of-pocket expenditure (OOPE) by Indian families (see World Bank figures). OOPE in India is ranked as one of the global highest with the major contributors being private healthcare service providers and cost of medicines. Before the pandemic, 55 million Indians were pushed annually below the poverty line due to such OOPE. In April 2020, India’s employment rate plummeted to 27% (vs 39% in April 2019) with a loss of 21 million salaried workers between April-August, invariably affecting the poorest.
The only way to access free or inexpensive health care in India is through the public health system, which can, unfortunately, cater to only about 30% of population needs at its current capacity. The COVID-19 burden was initially borne by the public hospitals; however, it negatively impacted the health service provision of non-COVID cases. Eventually, with incapacitated and overcrowded public hospitals, most of the large private hospitals also started providing COVID-19 treatment. The private hospitals and laboratories notoriously capitalized on the services provided and initially charged about USD60 for Sars-CoV-2 testing, USD1400 per day for ICU occupancy, and USD110 for ambulance services in some Indian states. Although the government later capped the price, these services remains a luxury for many. While the Out-patient department continue to be under-utilised, In-patient department (IPD) fees for all illnesses have increased due to the mandatory use of personal protective equipment (PPE). Moreover, some private hospitals have been accused of charging disproportionately inflated prices for PPE leading to remarkably high medical bills. The failure of many private insurers to cover the cost of PPE for IPD hospitalizations, means that families must bear this cost.
Has the government found a solution?
Clearly not. The national health protection scheme of India, still in its infancy, is attempting to cover COVID-19 testing and treatment for families registered below poverty-line. However, the number of beneficiaries availing these services are not publicly disclosed. These numbers are likely to be very low given the poor utilization of scheme in the empanelled large private hospitals where the hospitalization costs could often be greater than the national health cover provided. This clearly indicates that most patients availing treatment for COVID-19, especially the ones with ICU or longer hospital stays, would pay hefty OOPE, many of whom would be unable to afford the cost. Consequently, the vulnerable may avoid utilising healthcare services, unless critical, due to the fear of CHE and abject deprivation (see this Journal of Public Health paper).
In effect, the financial cover, especially for those visiting private hospitals for COVID-19 treatment, has not been thought well by the government. Like India, many low- and middle-income countries (LMICs) are facing a similar challenge and this is a significant issue to have been overlooked by the mainstream global health discourse.
The way forward
The financial burden related to COVID-19 treatment can bar many families to seek care and can be an important reason for poor containment of the pandemic. This can lead to an excess wage loss, morbidity and mortality resulting in a vicious cycle of economic loss and a rising inequality. We hence argue that the governments should cover the COVID-19 treatment costs and offer financial protection to families at risk of CHE. Essentially, the governments should regulate and provide cover for OOPs incurred on direct and indirect costs of COVID-19 care such as transport, wage loss, OPD expenses, indoor expenses, tests, and medicines etc., while continuing the search for the highly contested vaccine and cure. The global health community must develop coherent strategies through necessary collaborations to mobilize resources and develop policies before many more of the everyday people are pushed towards or into poverty. The poor are already facing the brunt of the pandemic due to overcrowded public hospitals resulting in delayed availability and sub-optimal level of care that cost lives. More research is thus required to understand the social determinants of COVID-19 transmission, including financial barrier to COVID-19 care, especially in the in low-resourced settings.