Source: World report on disability: www.who.int/disabilities/world_report
Disability-inclusive health systems in fragile & shock-prone settings
24 February 2021
People with disabilities continue to be underserved by health systems in low- and middle-income countries and their health care needs are largely unmet. In this blog Lynda Keeru, on behalf of Pamoja Communications, summarises a series of presentations from a ReBUILD for Resilience webinar on disability-inclusive health systems.
Setting the scene
15% of the world’s population is thought to have a disability and their health needs are three-fold; this population has the same health needs as everybody else but is also more vulnerable to poor health and may also require specialised medical treatment or rehabilitation services.
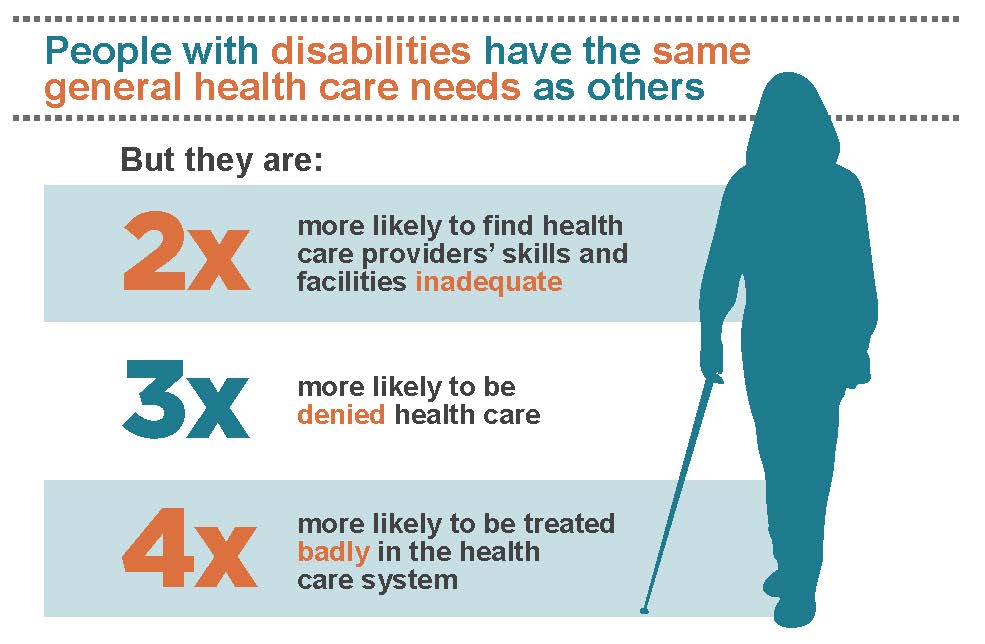
According to the World Health Organization (see their infographic here), people with disabilities are twice as likely to find health care providers’ skills and facilities inadequate, three times more likely to be denied health care and four times more likely to be treated badly in the health care system. This community is all too frequently left to suffer health disparities due to cultural incompetence, stigma and discrimination, and an inability to create policy changes that cover the population as a whole and their acute and long-term needs.
Studies indicate that overall mortality rates for people living with disabilities are two to three times higher for people living in Africa. In the event of a pandemic like COVID-19, people living with disabilities are more vulnerable. For example, according to Hannah Kuper at London School of Hygiene and Tropical Medicine, 59% of UK COVID-19 deaths were recorded among the 16% of the population living with a disability.
Research on disability is often siloed from other areas of health because there is a serious lack of data on both the people living with disabilities and their priority issues. It also has a lot to do with funding, cultural/historic practices and how government ministries are set up. Disability services also compete for funds and resources with other programmes that are considered more important. In fragile and shock-prone settings mobilisation of resources is also immensely challenging.
Providing solutions for disability-inclusive health systems
We need to collect best practice on the work being done in the realm of disability to learn from each other and to see how these successes can be replicated across different settings. People with disabilities and the organisations that represent them are key to identifying these best practices the health system and should also be involved in research and policy priority setting.
In order to improve this situation, solutions need to tackle health system challenges like the lack of health provider infrastructure and capacity, and improve health worker knowledge. The care workers of disabled people are usually unpaid or under-paid and not taken care of which also needs to change. Their working conditions need to be improved and psychosocial support should be provided.
It is vital that we acknowledge that the health disparities disabled people face are far less about people’s disabilities and much more to do with society’s inability to design social and health care frameworks to enable people to function optimally. Policy changes supported by accurate and sufficient data – which is currently lacking – should contribute to such much needed change. In order to mainstream disability, it must be included as a priority in all government ministries including health, education, finance etc. Building disability-inclusive health systems is a ‘whole-of-government’ endeavour.
Activist organisations have a key role to play in the lives of people living with disabilities and with pressing for this much-needed change. This includes highlighting the stories of disabled people. These organisations can also provide friendship and intimacy for this population that has suffered deep isolation and by so doing, help them forge much-needed connections and spark ideas for collective action.
In order to address the problems at the heart of our health systems, people living with disabilities must be involved in research processes right from the start, helping to identify priorities. Study designs should be inclusive and must utilise creative methodologies to support inclusion and dialogue at every level and to create disability-inclusive health systems.
Speakers
• Kyu Kyu Than (Chair) – Burnet Institute Myanmar
• Joanna Raven – Liverpool School of Tropical Medicine, UK
• Hannah Kuper – London School of Hygiene and Tropical Medicine, UK
• Nukhba Zia – Johns Hopkins Bloomberg School of Public Health, USA
• Aicha Benyaich – International Committee of the Red Cross, Lebanon
• Deepak Raj Sapkota – Karuna Foundation, Nepal
• Laura Dean – Liverpool School of Tropical Medicine, UK
• Janet Price – Activist, scholar, DadaFest, honorary research fellow at LSTM
Further information
A full recording of this session, with subtitles, can be viewed here.