Climate resilient health systems: Framework of action
How can we make health systems in Pakistan more climate resilient?
31 July 2023
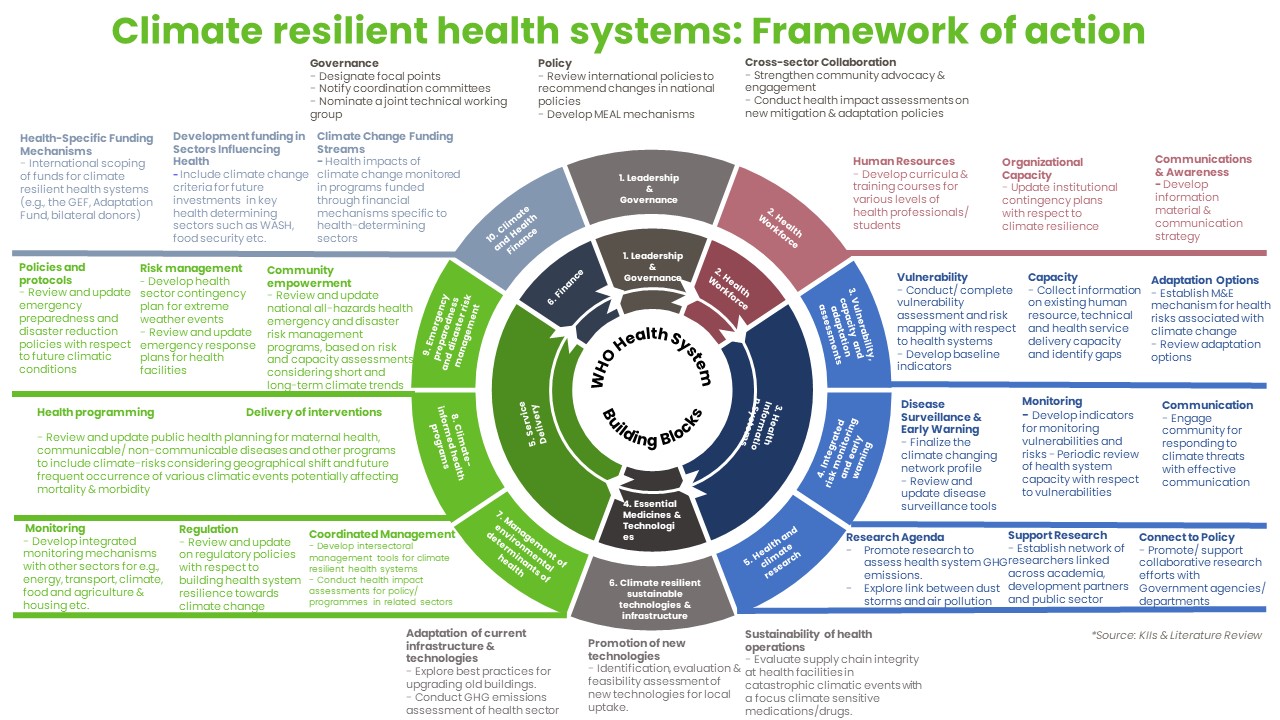
NB A text version of the above diagram can be read here
After attending COP26, the Pakistani Ministry of National Health Services, Regulation, and Coordination (M/o NHSRC) recognised the need for urgent work to address the effects of climate change on human health. The Director General of Health consequently commissioned a scoping study to understand existing work on climate resilient health systems in Pakistan. Oxford Policy Management (OPM) Pakistan [opens new tab] undertook this scoping study for the M/o NHSRC, as part of an ongoing technical assistance programme funded by the UK Foreign and Commonwealth Development Office (FCDO). In this blog post, Dr Mahwish Hayee [opens new tab] of OPM explains the need to strengthen resilience of health systems to climate change in Pakistan and summarises the study’s findings, providing a roadmap of action for next steps.
Did you know that Pakistan ranks as the fifth-most climate-vulnerable country in the world? [see the Global Climate Risk Index – opens new tab] Pakistanis are already feeling the brunt of climate change through devastating floods, melting glaciers, extreme temperatures, heavy monsoon downpours, and landslides [see Fahad & Wang, 2019 – opens new tab]. With the situation worsening in the country, it is essential to assess the capacity of health systems to respond to and adapt to climate risks, protect public health, and recover from climate-related events.
Pakistan’s aspirations to abide by the COP26 objectives
The recently concluded 26th United Nations Climate Change Conference of the Parties (COP26) presented an opportunity to boost global efforts to mitigate and prevent climate change. COP26 called for countries to establish climate-resilient health systems that consider current and future climate projections. This is crucial for safeguarding the health of populations against the impacts of climate change (see Lancet Countdown on Health & Climate Change 2022 – opens new tab]. More than 60 countries, including Pakistan, committed to the five primary objectives agreed at COP26 [opens new tab] to address the intersection of climate change and public health:
1. Deepening adaptation research for health
2. Building climate-resilient health systems
3. Developing low-carbon sustainable health systems
4. Including health priorities in Nationally Determined Contributions (NDCs)
5. Raising the voice of health professionals as advocates for stronger ambition on climate change
Our assessment of climate resilience in Pakistan’s health policies
To support progress towards climate resilience in Pakistan, FCDO commissioned research to identify the major gaps and weaknesses in policies and programmes essential to climate-resilient health systems, and to propose a framework of action [download the framework here] to accelerate progress toward a greener, more adaptive, and resilient health system. The study was an initial starting point to engage relevant stakeholders and initiate a discussion on how best to make progress. To assess the extent of climate resilience in health policies, planning, and implementation in Pakistan, we conducted a rapid review of grey and published literature, and a series of key informant interviews. The World Health Organization’s (WHO) Operational Framework for Building Climate Resilient Health Systems [opens new tab] served as the analytical and organising framework for the review. The framework provides guidance for health systems and public health programmes to bolster capacity in making health systems more climate shock responsive and suggests areas for action across the health system building blocks.
Our findings and moving forward
Our review identified significant gaps that could be addressed to meet Pakistan’s commitments on climate resilience. Here are our key findings:
- Governance and leadership: There are weaknesses in Leadership and governance for building climate-resilient health . For example, there are few effective fora for cross-sector discussion to enable coordination between government ministries and departments, and leadership is constrained by a lack of focal points for work on climate change and health. Reflecting and contributing to the lack of leadership and action, there is little mention of climate resilience in national health policy and planning documents, and , little mention of health in climate-related policies.
- Human resources for health: there is limited awareness among health policy makers and the wider health workforce about the links between climate change and health or about how to strengthen climate-resilience. This contributes to the lack of leadership around climate resilience. Some recent initiatives to develop courses on climate change and health in Pakistan provide opportunities for future capacity development.
- Health information systems: information systems do not currently provide adequate data on climate-related risks to inform health planning. There are not effective systems to share meteorological information on current and future climate hazards with health facilities or other health departments, health facilities lack guidelines on how to use climate change forecasts to detect long-term risks, and early warning systems and advisories for climate hazards are not currently operating effectively. The disease surveillance system does not adequately capture climate-sensitive health risks, and where climate-related conditions are tracked (such as heat-related death), this information is siloed rather than being integrated into wider disease surveillance and health management information.
- Infrastructure and technology: there is very little information on the contribution of Pakistan’s health system to greenhouse gas emissions, or on the effects of climate extremes on health infrastructure. In terms of regulation, there are guidelines on environmental standards for construction of new public sector buildings, but implementation remains a challenge. In addition, much health infrastructure is old, and many health facilities are in the private sector. The limited existing information points to the need for action on waste management (a key source of emissions), and to the potential role of digital technologies and renewable energy for health facilities. Renewable sources could be a ‘win-win’ option, providing more stable electricity for facility cold chains as well as a reducing fossil fuel use.
- Financing: Pakistan currently lacks integrated information on climate financing. There has been little focus on accessing funds to address climate resilience in health, partly due to the lack of technical capacity and leadership noted above. Previous programmes that strengthened capacity to access climate change funds and new funding sources that aim to promote climate change-related interventions provide opportunities for future funding.
- Service delivery: climate change has multiple current and potential effects on health service delivery and the disease burden in Pakistan, including changes in communicable and non-communicable diseases, as well as issues such as internal migration. These climate effects have not yet been translated into health programme planning. Emergency preparedness systems do not adequately consider current or future climatic risks, focusing only on major events such as floods and earthquakes, and disaster management tends to be reactive rather than proactive in responding to climate-induced disasters.
- Research and data on climate-resilient health systems: climate change and health is a neglected area of research in Pakistan, and current research efforts are disjointed. For example, the review could not find published data on well-defined climate indicators in Pakistan and their linkages with existing health surveillance systems, and there was little research on how best to reduce greenhouse gas emissions in the health sector in Pakistan, or on the health effects of climate-related interventions (such as changing fuel sources or reducing fossil fuel subsidies). The financial costs of climate change for the health sector, existing financing and the costs of strengthening health system resilience are a particular evidence gap.
Our recommendations: a proposed roadmap for action
To address these findings, we proposed a framework of action [download the framework here] to propel progress towards a climate resilient health system. Here are our recommendations:
- Improve leadership and governance for building climate-resilient health systems, including by designating focal points for climate change and health; developing a steering mechanism for collaboration and coordination between ministries and sectors; integrating climate change in key health policies; developing monitoring, evaluation and accountability mechanisms; and increasing use of data on climate and health in decision making.
- Build the capacity of current and future health workers to address climate change-related health risks through training courses and effective communication strategies.
- Conduct multisectoral assessments of climate vulnerability and adaptation of the national health system in Pakistan.
- Integrate environmental indicators like extreme weather or precipitation warnings into early warning systems for disease surveillance to detect near-term health risks.
- Identify feasible and effective uses of low-carbon, energy-efficient and climate-smart technology, assess options for upgrading/retrofitting existing health infrastructure to enhance resilience, including renewable energy for health facilities, and identify ways to reduce emmissions in the medical supply chain.
- Increase funding for climate resilience by submitting proposals related to health system to international climate change funds, and integrating climate change considerations in proposals for health projects (including to major global funds that address climate-sensitive diseases, such as the Global Fund to Fight AIDS, Tuberculosis and Malaria).
- Leverage funding for health system resilience through collaboration between the M/o NHSC&Research and the National Disaster Risk Management Fund (NDRMF), which manages a pool of international funds earmarked for climate change-induced risks and vulnerability, as well as with the Ministry of Climate Change, a key implementation agency for this fund.
- Evaluate the costs that may arise from inaction, as information on the economic impact of climate-related health risks could serve as a strong motivator to accelerate climate change mitigation and resilience efforts in the health sector and beyond.
- Review and update public health programme planning to include climate risks, for integrated health programmes, communicable and non-communicable diseases and other programme areas.
- Include climate change as a risk factor in emergency planning and preparedness, using data on expected health impacts.
- The research community should prioritise work on climate change and health to inform policy and implementation, and strengthen capacity and research uptake via networks and communities of practice on climate-resilient health systems. Among other areas, research needs include a greenhouse gas inventory for health systems to track emissions annually, and evidence on the potential or expected health impacts of climate-related interventions.
To sum up…
Pakistan faces significant challenges due to climate change, affecting the health and well-being of its people. By adopting the proposed roadmap for action, we can move towards a resilient health system that effectively responds to climate risks and protect lives. It is crucial to prioritise climate resilience in health policies, strengthen leadership, enhance research efforts, and invest in sustainable technologies. Together, we can navigate the challenges of climate change and ensure a healthier, more secure future for Pakistan’s population.